|
Case Report
Atypical manifestations in children with Guillain–Barré syndrome
1 Medical Sciences Course, Health Sciences School, Faculdade Ceres (FACERES), São José do Rio Preto, SP, Brazil
2 Neurosurgeon, Member of the Brazilian Society of Neurosurgery, Santa Mônica Hospital, Goiânia, GO, Brazil
3 Neurosurgeon, PhD in Neurosurgery, Member of the Brazilian Society of Neurosurgery, Professor at Santa Mônica Hospital, Goiânia, GO, Brazil
Address correspondence to:
Julia Brasileiro de Faria Cavalcante
Rua T38, 1097, Setor Bueno, apt 601, Goiânia, GO,
Brazil
Message to Corresponding Author
Article ID: 100014N06JC2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Cavalcante JBF, Cembraneli PN, Cavalcante RBF, Junior VFV, Cavalcante JES. Atypical manifestations in children with Guillain–Barré syndrome. Edorium J Neurol 2020;7:100014N06JC2020.ABSTRACT
Introduction: Guillain–Barré syndrome (GBS) is an acute single-phase inflammatory demyelinating polyneuropathy that occurs after an infection, characterized by a clinical pattern of acral paresthesias, ascending generalized weakness, and areflexia. Its worldwide incidence ranges from 0.5 to 1.5/100,000 children/year, predominantly males. In children, the predominant symptoms are vague paresthesias, significant, poorly localized pain, weakness manifesting as disturbance of gait, and cranial nerve abnormalities, with facial nerves most commonly affected.
Case Report: A 13-month-old female patient, crying for five days, presented with low fever, progressive, asymmetric loss of strength in lower limbs, regular general condition, tachypnea, tachycardia, hypotonia of right upper limb and left lower limb, positive Babinski sign to the right, Achilles and patellar tendon areflexia, discreet neck stiffness, hypoesthesia, and pain from the lower limbs to the xiphoid process, leading to the diagnosis of GBS. The cerebrospinal fluid did not indicate any alterations and the electroneuromyography showed reduced motor unit action potentials and normal motor conduction velocity, revealing acute motor axonal neuropathy. The patient developed respiratory arrest, requiring intensive care therapy, and orotracheal intubation. Immunoglobulin therapy was initiated and the patient gradually recovered the movements and reflexes.
Conclusion: It is very important to point out that when GBS is suspected, even if it is atypical, the patient should be admitted to the pediatric intensive care unit. This allows intensive nursing care and continuous monitoring to reduce the frequency and severity of complications.
Keywords: Asymmetry, Guillain–Barré syndrome, Paresthesia
INTRODUCTION
Guillain–Barré syndrome (GBS) is classified as an eponym that encompasses acute immune-mediated polyneuropathies. It is considered to be an acute monophasic paralyzing disease that usually occurs after an infection and the most common cause of flaccid paralysis in the world [1],[2],[3]. Its worldwide incidence ranges from 0.89 to 1.89/100,000 people/year (average 1.1) and, more specifically, 0.5 to 1.5/100,000 children/year, predominantly affecting males. Although all age bands may be affected, the peak incidence ranges from 20 to 40 years, with an increase of approximately 20% every ten years after the first decade of life [1],[4],[5],[6].
The clinical presentation of GBS begins with paresthesias in the hands and feet, followed by progressive symmetrical muscle weakness, which begins in the lower limbs and may last hours or even months [1],[4],[5]. In children, proximal weakness is less common, whereas pain and difficulty in gait and greater involvement of cranial pairs predominate [7],[8],[9]. In approximately 70% of the cases, patients had a previous infection about 1–3 weeks before. Generally, this infectious condition was of gastrointestinal or respiratory origin and the most common etiological agents are: Campylobacter jejuni, cytomegalovirus, and Epstein–Barr virus. The first agent is frequently associated with the most severe type of this syndrome, the acute motor axonal neuropathy (AMAN) [10].
Guillain–Barré syndrome has four presentations, here listed from the most to the least common: acute demyelinating inflammatory polyneuropathy (AIDP), AMAN, Miller–Fischer syndrome, and acute motor and sensory axonal neuropathy. Acute demyelinating inflammatory polyneuropathy corresponds to 85–95% of cases, while AMAN represents 10–20% of them [1].
The diagnosis is primarily clinical. However, complementary exams such as cerebrospinal fluid (CSF) analysis and electroneuromyography (ENMG) are necessary to confirm the diagnostic hypothesis and rule out other causes of flaccid paraparesis [1],[3],[11]. After the diagnosis is confirmed, the treatment with immunoglobulin or plasmapheresis is initiated together with motor physical therapy [1],[12].
In general, the prognosis for children is better compared to that for adults, since approximately 85% of the pediatric patients have an excellent recovery [13]. Nonetheless, a small number of the children affected may be incapacitated or even progress to sepsis, pulmonary embolism, and death [1],[7].
Thus, we report a case of a 13-month-old female patient diagnosed with GBS, but with atypical clinical presentation and exam results.
CASE REPORT
A 13-month-old female patient was born by Caesarean section at 38 gestational weeks and 4 days, 3080 g, 47 cm, uneventful pregnancy and delivery, prenatal tests performed correctly. The baby was exclusively breastfed and walked at one year of age. She was referred to our service due to a history of low fever, accompanied by flu symptoms and crying for five days. She presented with progressive asymmetric loss of strength in lower limbs and cough. Given that she was followed up by a neurologist because of a diagnosis of macrocephaly since the age of six months, a magnetic resonance imaging (MRI) of the skull was carried out but showed no alterations.
The child evolved to a regular general state, with high respiratory rate (80 breaths per minute), characterizing tachypnea, associated with tachycardia (185 beats per minute), with ascending hypotonia of right upper limb and left lower limb. In addition, she cried constantly and presented with coldness to touch in the left lower limb.
The patient was examined by a neurosurgery team, who observed that she had axial and bilateral lower limb hypotonia, positive Babinski sign to the right, Achilles and patellar tendon areflexia, discreet neck stiffness, and hypoesthesia and pain from the lower limbs to the xiphoid process. The diagnosis of GBS was proposed based on two diagnostic criteria, namely progressive weakness in more than one limb and hyporeflexia/areflexia.
The examination of CSF revealed no protein increase, negative cultures, normal glucose level, and increased cellularity. The patient underwent ENMG to confirm the diagnostic hypothesis. This exam detected reduced motor unit action potentials and normal motor conduction velocity, indicating acute motor axonal neuropathy. The patient developed respiratory arrest, requiring intensive care therapy, and orotracheal intubation. She was intubated for 10 days and simultaneously underwent immunoglobulin therapy. She had improvements in the respiratory condition and showed gradual recovery of movements and reflexes. After being discharged from the intensive care unit (ICU), the patient remained hospitalized under the care of a neurologist and a pediatrician.
DISCUSSION
Guillain–Barré syndrome was first described in 1916 by the French neurologists Guillain, Barré, and Strohl, who reported the cases of two soldiers who developed acute paralysis with muscle weakness, areflexia, and albuminocytologic dissociation in the CSF [14]. Since polio eradication, GBS has become the most frequent cause of acute and subacute flaccid paralysis in the world [15],[16],[17].
Approximately 70% of GBS cases appear about 1–3 weeks after an infection, either respiratory, gastrointestinal, or any other type that induces an aberrant autoimmune response. Given that it is benign, most often this infection might be minimized or forgotten by the patient [16],[17],[18],[19]. The most widely reported agent is C. jejuni, but other infections associated with this condition are those caused by cytomegalovirus, Epstein–Barr virus, Measles morbillivirus, influenza virus, Mycoplasma pneumoniae, as well as enterovirus D68 and Zika virus [20],[21],[22],[23],[24],[25],[26],[27],[28].
One of the hallmarks of GBS is progressive, bilateral, ascending weakness that usually begins in the lower distal extremities but may begin more proximally in the lower and upper limbs, giving the false impression of a pyramidal lesion [29],[30],[31],[32]. Weakness peaks can take place within 2–4 weeks after the onset of symptoms and a small number of patients have paraparesis [32]. In addition, patients may initially have sensory signs, ataxia, and characteristic autonomic dysfunction. Approximately one-third of the patients have muscle or nerve root pain even before they develop weakness [33]. Most patients present with reduced tendon reflexes in the affected limbs that were initially normal [34]. This syndrome may progress for up to six weeks after its onset. About 20–30% of the patients develop complications and may require mechanical ventilation during the course of the illness [29].
Regarding the pathogenesis of this disease, for many years its severity was related to the extent of axonal lesion due to demyelination. However, it is currently known that several phenotypes, such as acute inflammatory demyelinating polyneuropathy, in which the injury related to the immune system attacks the myelin sheath, in addition to acute axonal motor neuropathy, when the axonal membranes are the main target [16]. Guillain–Barré syndrome generally affects healthy people and is not associated with an autoimmune disease or another systemic disorder. The assumption that GBS is primarily a T cell-mediated disease has been challenged by the discovery of anti-glycolipid Abs in GBS variants and chronic dysimmune neuropathies [35].
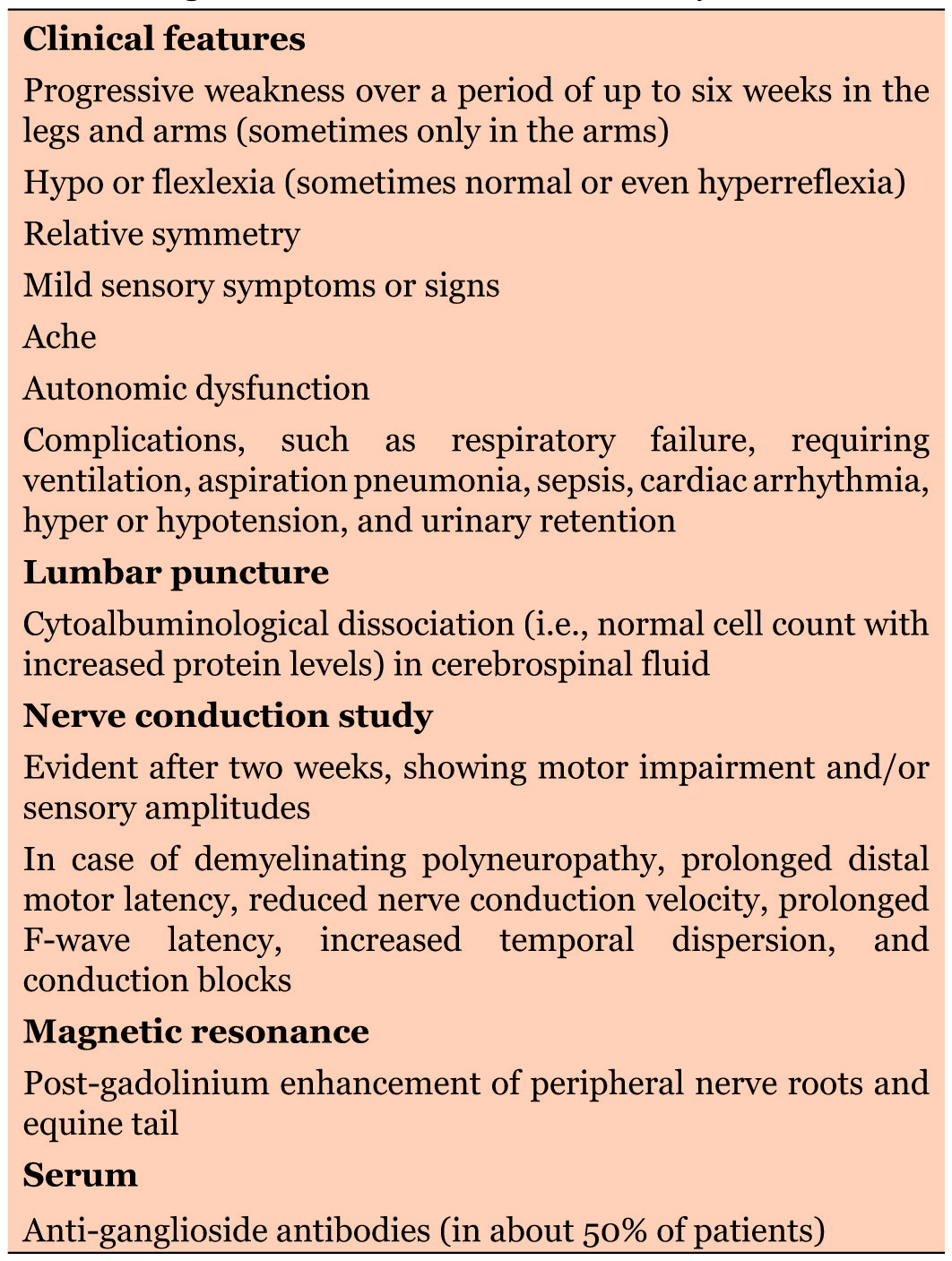
It can be difficult to diagnose GBS in young children because their complaints are frequently atypical and their neurological examination is more challenging [36]. Table 1 summarizes GBS diagnostic criteria based on clinical exams, although additional examinations may be required [13]. In general, the exclusion diagnosis is based on two main tests, CSF evaluation and ENMG. In the first, the combination of high CSF protein level and CSF cell count within normal limits (known as albuminocytological dissociation) points to a GBS diagnosis. In the second, demyelinating or axonal neuronal lesions indicate GBS [1],[11]. Although not specific, post-gadolinium enhancement of the anterior and the posterior nerve roots of cauda equina can be seen on MRI in up to 95% of the patients presenting with GBS [37],[38].
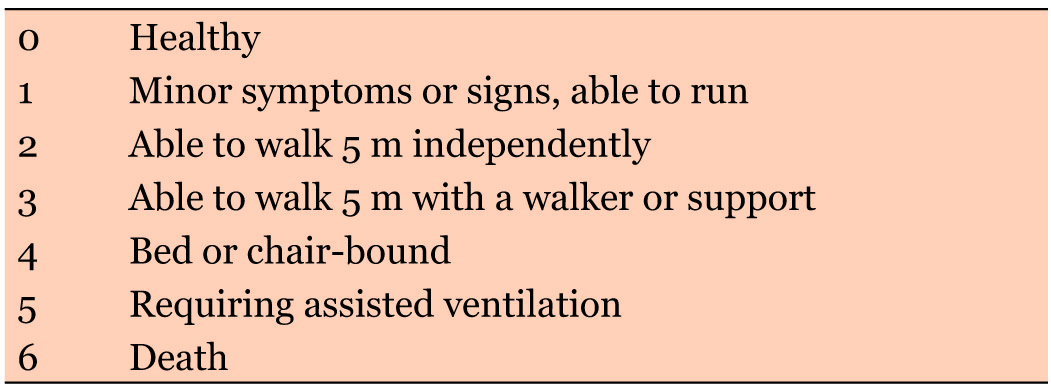
The neurological examination helps the diagnosis, since symmetrical weakness of the lower limbs with decreased or absent osteotendinous reflexes and neuropathic pain are frequently found in patients with GBS. Hughes functional grading scale for GBS (Table 2) is used to assess patients’ motor impairment [39].
In general, GBS is a life-threatening disease, with a mortality rate of 3–7% [40],[41]. Higher prevalence of death is due to ventilatory insufficiency, complications, or autonomic dysfunction [42]. Patients show improvement mainly within one year from GBS onset [43]. Worst outcomes are usually associated with older age (>40 years), diarrhea, or C. jejuni infection in the four weeks preceding the disease [16].
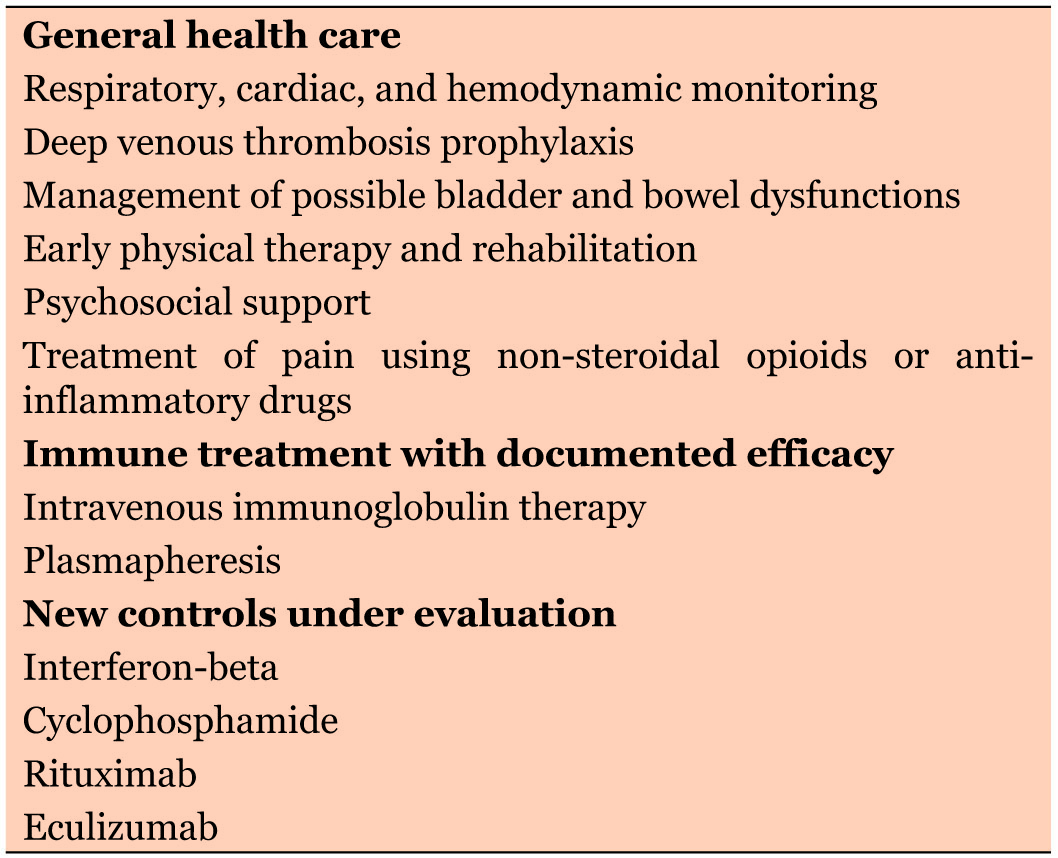
Treatment requires a multidisciplinary approach consisting of general medical care in addition to immunological treatment (Table 3). Respiratory, cardiac, and hemodynamic functions should be monitored, and complications should be prevented or treated [16]. For pain control, the use of non-steroidal opioids or anti-inflammatories is recommended [44]. Although no specific drug has been endorsed for the treatment of GBS, various drugs have been used to target the components of the immune response. Immunomodulatory treatments with immunoglobulin or plasmapheresis have been shown to be effective in accelerating recovery from GBS in addition to improving outcomes [1],[45].
CONCLUSION
It is very important to emphasize that if a diagnosis of GBS is suspected, even in atypical presentations, the child should be admitted to a pediatric ICU, under the care of a neurologist and a pediatrician, as the child of the present case report. The patients should remain there, inasmuch as they require continuous monitoring of hemodynamic and ventilatory parameters to provide life support, reduce the frequency and severity of complications, and detect autonomic changes early.
REFERENCES
1.
2.
Kieseier BC, Hartung HP. Therapeutic strategies in the Guillain-Barré syndrome. Semin Neurol 2003;23(2):159–68. [CrossRef]
[Pubmed]

3.
Vucic S, Kiernan MC, Cornblath DR. Guillain-Barré syndrome: An update. J Clin Neurosci 2009;16(6):733–41. [CrossRef]
[Pubmed]

4.
Erazo Torricelli R. Guillain Barré Syndrome in pediatrics. [Article in Spanish]. Medicina (B Aires) 2009;69(1 Pt 1):84–91.
[Pubmed]

5.
McGrogan A, Madle GC, Seaman HE, de Vries CS. The epidemiology of Guillain-Barré syndrome worldwide. A systematic literature review. Neuroepidemiology 2009;32(2):150–63. [CrossRef]
[Pubmed]

6.
Dourado ME, Félix RH, da Silva WK, Queiroz JW, Jeronimo SM. Clinical characteristics of Guillain-Barré syndrome in a tropical country: A Brazilian experience. Acta Neurol Scand 2012;125(1):47–53. [CrossRef]
[Pubmed]

7.
Lee JH, Sung IY, Rew IS. Clinical presentation and prognosis of childhood Guillain-Barré syndrome. J Paediatr Child Health 2008;44(7–8):449–54. [CrossRef]
[Pubmed]

8.
9.
Korinthenberg R, Schessl J, Kirschner J, Mönting JS. Intravenously administered immunoglobulin in the treatment of childhood Guillain-Barré syndrome: A randomized trial. Pediatrics 2005;116(1):8–14. [CrossRef]
[Pubmed]

10.
Monteiro JP, Fonseca S, Proenca J, Calhau P, Braga M, Fonseca MJ. Pediatric Guillain-Barré syndrome. Experience in the neuropediatrics unit of a Portuguese hospital. [Article in Spanish]. Rev Neurol 2006;42(3):144–9.
[Pubmed]

11.
Li S, Yu M, Li H, Zhang H, Jiang Y. IL-17 and IL-22 in cerebrospinal fluid and plasma are elevated in Guillain-Barré syndrome. Mediators Inflamm 2012;2012:260473. [CrossRef]
[Pubmed]

12.
Schleicher GK, Black A, Mochan A, Richards GA. Effect of human immunodeficiency virus on intensive care unit outcome of patients with Guillain-Barré syndrome. Crit Care Med 2003;31(6):1848–50. [CrossRef]
[Pubmed]

13.
Ryan MM. Pediatric Guillain-Barré syndrome. Curr Opin Pediatr 2013;25(6):689–93. [CrossRef]
[Pubmed]

14.
15.
Sejvar JJ, Baughman AL, Wise M, Morgan OW. Population incidence of Guillain–Barré syndrome: A systematic review and meta-analysis. Neuroepidemiology 2011;36(2):123–33. [CrossRef]
[Pubmed]

16.
Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet 2016;388(10045):717–27. [CrossRef]
[Pubmed]

17.
Esposito S, Longo MR. Guillain-Barré syndrome. Autoimmun Rev 2017;16(1):96–101. [CrossRef]
[Pubmed]

18.
van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain-Barré syndrome: Pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol 2014;10(8):469–82. [CrossRef]
[Pubmed]

19.
Walgaard C, Lingsma HF, Ruts L, van Doorn PA, Steyerberg EW, Jacobs BC. Early recognition of poor prognosis in Guillain–Barré syndrome. Neurology 2011;76(11):968–75. [CrossRef]
[Pubmed]

20.
Jasti AK, Selmi C, Sarmiento-Monroy JC, Vega DA, Anaya JM, Gershwin ME. Guillain-Barré syndrome: Causes, immunopathogenic mechanisms and treatment. Expert Rev Clin Immunol 2016;12(11):1175–89. [CrossRef]
[Pubmed]

21.
Loshaj-Shala A, Regazzoni L, Daci A, et al. Guillain Barré syndrome (GBS): New insights in the molecular mimicry between C. jejuni and human peripheral nerve (HPN) proteins. J Neuroimmunol 2015;289:168–76. [CrossRef]
[Pubmed]

22.
Orlikowski D, Porcher R, Sivadon-Tardy V, et al. Guillain-Barré syndrome following primary cytomegalovirus infection: A prospective cohort study. Clin Infect Dis 2011;52(7):837–44. [CrossRef]
[Pubmed]

23.
Tselis AC. Epstein-Barr virus infections of the nervous system. Handb Clin Neurol 2014;123:285–305. [CrossRef]
[Pubmed]

24.
Hawken S, Kwong JC, Deeks SL, et al. Simulation study of the effect of influenza and influenza vaccination on risk of acquiring Guillain-Barré syndrome. Emerg Infect Dis 2015;21(2):224–31. [CrossRef]
[Pubmed]

25.
Ghaderi S, Gunnes N, Bakken IJ, Magnus P, Trogstad L, Håberg SE. Risk of Guillain-Barré syndrome after exposure to pandemic influenza A(H1N1)pdm09 vaccination or infection: A Norwegian population-based cohort study. Eur J Epidemiol 2016;31(1):67–72. [CrossRef]
[Pubmed]

26.
Meyer Sauteur PM, Huizinga R, Tio-Gillen AP, et al. Mycoplasma pneumoniae triggering the Guillain-Barré syndrome: A case-control study. Ann Neurol 2016;80(4):566–80. [CrossRef]
[Pubmed]

27.
Williams CJ, Thomas RH, Pickersgill TP, et al. Cluster of atypical adult Guillain-Barré syndrome temporally associated with neurological illness due to EV-D68 in children, South Wales, United Kingdom, October 2015 to January 2016. Euro Surveill 2016;21(4). [CrossRef]
[Pubmed]

28.
Cao-Lormeau VM, Blake A, Mons S, et al. Guillain-Barré syndrome outbreak associated with Zika virus infection in French Polynesia: A case-control study. Lancet 2016;387(10027):1531–9. [CrossRef]
[Pubmed]

29.
Fokke C, van den Berg B, Drenthen J, Walgaard C, van Doorn PA, Jacobs BC. Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain 2014;137(Pt 1):33–43. [CrossRef]
[Pubmed]

30.
Sejvar JJ, Kohl KS, Gidudu J, et al. Guillain-Barré syndrome and Fisher syndrome: Case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine 2011;29(3):599–612. [CrossRef]
[Pubmed]

31.
van Doorn PA. Diagnosis, treatment and prognosis of Guillain-Barré syndrome (GBS). Presse Med 2013;42(6 Pt 2):e193–201. [CrossRef]
[Pubmed]

32.
van den Berg B, Fokke C, Drenthen J, van Doorn PA, Jacobs BC. Paraparetic Guillain-Barré syndrome. Neurology 2014;82(22):1984–9. [CrossRef]
[Pubmed]

33.
Ruts L, Drenthen J, Jongen JL, et al. Pain in Guillain-Barré syndrome: A long-term follow-up study. Neurology 2010;75(16):1439–47. [CrossRef]
[Pubmed]

34.
Yuki N, Kokubun N, Kuwabara S, et al. Guillain-Barré syndrome associated with normal or exaggerated tendon reflexes. J Neurol 2012;259(6):1181–90. [CrossRef]
[Pubmed]

35.
Soliven B. Animal models of autoimmune neuropathy. ILAR J 2014;54(3):282–90. [CrossRef]
[Pubmed]

36.
Roodbol J, de Wit MC, Aarsen FK, Catsman-Berrevoets CE, Jacobs BC. Long-term outcome of Guillain-Barré syndrome in children. J Peripher Nerv Syst 2014;19(2):121–6. [CrossRef]
[Pubmed]

37.
Yikilmaz A, Doganay S, Gumus H, Per H, Kumandas S, Coskun A. Magnetic resonance imaging of childhood Guillain-Barre syndrome. Childs Nerv Syst 2010;26(8):1103–8. [CrossRef]
[Pubmed]

38.
Zuccoli G, Panigrahy A, Bailey A, Fitz C. Redefining the Guillain-Barré spectrum in children: Neuroimaging findings of cranial nerve involvement. AJNR Am J Neuroradiol 2011;32(4):639–42. [CrossRef]
[Pubmed]

39.
Chand P, Jan F, Kaleem S, Yousafzai MT, Ibrahim S. Description of Guillain-Barre syndrome on the basis of clinical features using Hughes scoring system among children in Karachi, Pakistan. Asia Pac J Clin Trials Nerv Syst Dis 2017;2:45–9. [CrossRef]

40.
Hughes RA, Swan AV, Raphaël JC, Annane D, van Koningsveld R, van Doorn PA. Immunotherapy for Guillain-Barré syndrome: A systematic review. Brain 2007;130(Pt 9):2245–57. [CrossRef]
[Pubmed]

41.
Živković S. Intravenous immunoglobulin in the treatment of neurologic disorders. Acta Neurol Scand 2016;133(2):84–96. [CrossRef]
[Pubmed]

42.
Darweesh SK, Polinder S, Mulder MJ, et al. Health-related quality of life in Guillain-Barré syndrome patients: A systematic review. J Peripher Nerv Syst 2014;19(1):24–35. [CrossRef]
[Pubmed]

43.
Leonhard SE, Mandarakas MR, Gondim FAA, et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat Rev Neurol 2019;15(11):671–83. [CrossRef]
[Pubmed]

44.
Ostronoff F, Perales MA, Stubblefield MD, Hsu KC. Rituximab-responsive Guillain-Barré syndrome following allogeneic hematopoietic SCT. Bone Marrow Transplant 2008;42(1):71–2. [CrossRef]
[Pubmed]

45.
Vitaliti G, Tabatabaie O, Matin N, et al. The usefulness of immunotherapy in pediatric neurodegenerative disorders: A systematic review of literature data. Hum Vaccin Immunother 2015;11(12):2749–63. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Julia Brasileiro de Faria Cavalcante - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Pedro Nogarotto Cembraneli - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Renata Brasileiro de Faria Cavalcante - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Volmer Fernandes Valente Junior - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
José Edison da Silva Cavalcante - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Julia Brasileiro de Faria Cavalcante et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.