|
Case Report
Anti-NMDA antibody autoimmune encephalitis post-HSV encephalitis: A rare case report
1 DrNB Neurology, Department of Neurology, Indraprastha Apollo Hospital, New Delhi, India
2 Professor/Senior Consultant, Department of Neurology, Indraprastha Apollo Hospital, New Delhi, India
3 Attending Consultant, Department of Neurology, Indraprastha Apollo Hospital, New Delhi, India
4 Senior Consultant, Department of Radiology, Indraprastha Apollo Hospital, New Delhi, India
Address correspondence to:
Pushpendra Nath Renjen
Professor/Senior Consultant, Department of Neurology, Indraprastha Apollo Hospital, New Delhi,
India
Message to Corresponding Author
Article ID: 100018N06NS2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sahu N, Renjen PN, Goswami A, Kanuga S, Goyal N. Anti-NMDA antibody autoimmune encephalitis post-HSV encephalitis: A rare case report. Edorium J Neurol 2024;9(1):1–4.ABSTRACT
Introduction: Autoimmune encephalitis is a group of neuropsychiatric disorder in which antibodies interact directly to their target antigen and produce neuronal dysfunction. Generally herpes simplex encephalitis is a monophasic illness although in few patients neurological worsening can develop some weeks later. This worsening is generally due to autoimmune encephalitis after herpes simplex encephalitis (AEaHSE).
Case Report: We report an interesting case report of 67 years old female patient who initially was diagnosed to have herpes simplex virus (HSV) encephalitis, showed improvement in her clinical status followed subsequently by deterioration in cognitive status. Anti-N-methyl-D-aspartate (NMDA) antibody was positive in cerebrospinal fluid (CSF) and serum. The patient was managed with intravenous immunoglobulin (IVIG) and subsequently showed improvement in her clinical state.
Conclusion: The discovery and clinical application of anti-NMDA receptor antibodies has helped to define the mechanism behind immune-based relapse of herpes simplex virus encephalitis (HSVE). This case illustrates the usefulness of testing for anti-NMDA receptor antibodies following worsening few weeks after treatment of herpes simplex encephalitis.
Keywords: Anti-NMDA encephalitis, Autoimmune, HSV encephalitis, Post-infection
INTRODUCTION
Herpes simplex encephalitis (HSE) is considered to be one of the most common sporadic viral encephalitis. It has an annual incidence of 2–4 cases per million people worldwide, accounting for almost 20% of all encephalitis cases [1]. Most HSEs occur in children and the elderly and in these age groups herpes simplex virus-1 (HSV-1) has the major etiologic role [2].
CASE REPORT
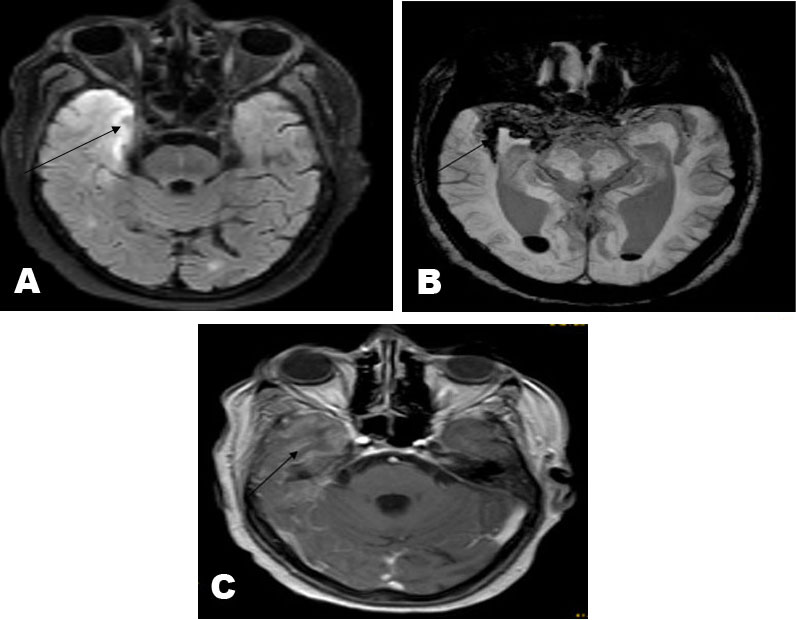
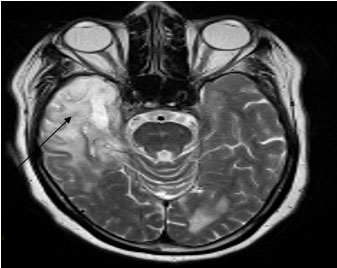
A 67-year-old female, hypertensive and diabetic, developed abnormal involuntary movements of left limbs with altered sensorium and had fever around the same time. The patient was admitted, where she was intubated and put on mechanical ventilation. Cerebrospinal fluid (CSF) examination revealed white blood cells (WBC) – few cells protein – 133, sugar – 132 [corresponding random blood sugar (RBS) 101], and CSF HSV-1 real-time polymerase chain reaction (RT-PCR) was positive. The patient was managed with antibiotics, antiviral, antiepileptic and other supportive care. She was drowsy, arousable intermittently follows simple commands, The pupils were symmetrical and reactive measuring 2 mm. Muscle strength in right upper and lower limb was 2/5 1/5 and left upper and lower limb was 2/5 1/5, plantars were extensor bilaterally. Magnetic resonance imaging (MRI) brain FLAIR (fluid-attenuated inversion recovery) revealed evidence of ill-defined area of altered signal intensity predominantly involving the medial temporal lobe, which is extending along the anterior temporal lobe and extending superiorly along the internal and external capsule. Signal intensity alteration is also seen involving the right-sided thalamus with relative sparing of the basal ganglia. Mild similar changes are also seen involving the left temporal lobe and the capsular region (Figure 1A). Focal area of parenchymal bleed is seen in the right medial temporal lobe. The hemorrhage is also seen extending into the subarachnoid spaces along the right sylvian fissure. Bleed is also seen in the dependent part of bilateral lateral ventricle with fluid level (Figure 1B). Abnormal leptomeningeal enhancement is seen involving the sylvian and perisylvian regions on both sides, more prominently on right side. Abnormal enhancement is also seen along the convexity sulcal spaces in the right temporal region and along the interhemispheric fissure (Figure 1C). These findings are likely secondary to HSV encephalitis. The patient gradually improved to a conscious and alert stage with moving all 4 limbs and obeying commands. She was discharged after one month of hospital stay. Subsequently, the patient was admitted with complaints of cognitive decline, irrelevant talking, and altered sensorium started one month after discharge. The patient was not following verbal commands and comprehension was also impaired. Follow-up MRI brain revealed ill-defined area of FLAIR hyperintensity involving the right anterior and medial temporal lobe with evidence of volume loss prominent in the anteromedial temporal lobe including thinning of the right hippocampus. Interspersed magnetic susceptibility is seen in the sylvian fissure and in the medial temporal lobe: suggestive of hemorrhagic residua. The signal changes are seen extending superiorly along the internal and external capsule and involving the right frontal lobe, right periventricular and deep white matter including the corona radiata and centrum semiovale (Figure 2). Compared to the previous MRI there is mild increase in the extent of the FLAIR hyperintensity with interval encephalomalacic changes in the right temporal lobe. Similar ill-defined signal changes were also seen in the left perisylvian region, the periventricular and deep white matter including left corona radiata and centrum semiovale with mild increase in the left periventricular hyperintensity compared to the previous study. Persisting ill-defined FLAIR hyperintensity was also seen involving the right-sided thalamus with relative sparing of the basal ganglia with no significant change. There is near complete resolution of the hemorrhagic residua seen in the dependent part of bilateral lateral ventricle in the previous study. Also, there is near complete resolution of the leptomeningeal enhancement seen in the previous study. The ventricular system is appearing mildly more prominent from the previous study. Lumbar puncture revealed CSF glucose-79 (RBS144), protein – 74.9, cells–5 with negative rapid meningitis panel, negative aerobic, anaerobic, fungal cultures, and negative gram, AFB, KOH, and India ink stains. Cerebrospinal fluid autoimmune encephalitis panel was positive for anti NMDA antibodies. Positron emission tomography-computed tomography (PET-CT) of the whole body revealed an ill-defined hypodense area involving the right temporal lobe with reduced F-fluorodeoxyglucose (FDG) uptake. Reduced uptake was also seen in bilateral periventricular regions and the right frontal lobe. The patient was managed with 140 grams of IVIG over a period of five days, antiepileptic drug and other supportive care. Subsequently she showed improvement in her neurological state and discharged in a hemodynamically stable condition.
DISCUSSION
N-methyl-D-aspartate receptor (NMDAR) encephalitis is an autoimmune encephalitis syndrome characterized by variable combinations of neuropsychiatric and behavioral changes, seizures, movement disorders, amnesia, aphasia, other neuropsychiatric symptoms and autonomic dysfunction [3]. Immunoglobulin G (IgG) antibodies to the NR1 subunit of the NMDAR contribute to pathogenesis and affect neuronal function [3]. A subset of patients with anti-NMDAR encephalitis has certain group of tumors, an ovarian teratoma, and pathogenesis in these cases is thought to be paraneoplastic [4]. In patients without tumors, the pathogenesis is generally assumed to be autoimmune [5],[6]. Early hypotheses for the mechanisms underlying post-HSVE-AE considered the possibility of molecular mimicry between HSV surface molecules and NMDARs [7]. Although the exact mechanisms underlying the synthesis of anti-NMDAR antibodies following HSV infection remain unknown, it is hypothesized that the virus induced neuronal destruction may expose neuronal antigens to the systemic immunity, initiating a primary autoimmune response [8]. In their important analysis, the authors describe 4 distinct imaging patterns in MRI brain: normal MRI findings (type 1, 53% of patients), isolated hippocampal involvement (type 2, 13%), other brain lesions without hippocampal involvement (type 3, 13%), and other brain lesions with hippocampal involvement (type 4, 21%) [9],[10].
CONCLUSION
The discovery and clinical application of anti-NMDA receptor antibodies has helped to define the mechanism behind immune based relapse of HSVE. This case illustrates the usefulness of testing for anti-NMDA receptor antibodies following worsening few weeks after treatment of herpes simplex encephalitis.
REFERENCES
1.
Esposito S, Autore G, Argentiero A, Ramundo G, Principi N. Autoimmune encephalitis after herpes simplex encephalitis: A still undefined condition. Autoimmun Rev 2022;21(12):103187. [CrossRef]
[Pubmed]

2.
Granerod J, Ambrose HE, Davies NW, et al. Causes of encephalitis and differences in their clinical presentations in England: A multicentre, population-based prospective study. Lancet Infect Dis 2010;10(12):835–44. [CrossRef]
[Pubmed]

3.
Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: An observational cohort study. Lancet Neurol 2013;12(2):157–65. [CrossRef]
[Pubmed]

4.
Planagumà J, Leypoldt F, Mannara F, et al. Human N-methyl D-aspartate receptor antibodies alter memory and behaviour in mice. Brain 2015;138(Pt 1):94–109. [CrossRef]
[Pubmed]

5.
Hacohen Y, Deiva K, Pettingill P, et al. N-methyl-D-aspartate receptor antibodies in post-herpes simplex virus encephalitis neurological relapse. Mov Disord 2014;29(1):90–6. [CrossRef]
[Pubmed]

6.
Brás A, André A, Sá L, et al. Anti-NMDAR encephalitis following herpes simplex virus encephalitis: 2 cases from Portugal. Neurohospitalist 2020;10(2):133–8. [CrossRef]
[Pubmed]

7.
Leypoldt F, Wandinger KP. Post-herpes simplex virus encephalitis autoimmunity: More the rule than the exception. Brain 2023;146(10):3963–5. [CrossRef]
[Pubmed]

8.
Prüss H, Finke C, Höltje M, et al. N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 2012;72(6):902–11. [CrossRef]
[Pubmed]

9.
Scheel M, Finke C. MRI findings suggestive of herpes simplex encephalitis in patients with anti-NMDA receptor encephalitis. AJNR Am J Neuroradiol 2018;39(11):E120. [CrossRef]
[Pubmed]

10.
Swayne A, Brown H, Singh G, Blum S. Anti-NMDA receptor encephalitis complicating HSV encephalitis with demonstrated serocon version. Journal of Neurology, Neurosurgery & Psychiatry 2017;88(5):e1. [CrossRef]

SUPPORTING INFORMATION
Author Contributions
Neelam Sahu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Pushpendra Nath Renjen - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Avinash Goswami - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shams Kanuga - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nidhi Goyal - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Neelam Sahu et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.